Seoul National University Hospital Develops AI Model to Simultaneously Predict Three Major Postoperative Complications
- Trained on data from more than 80,000 surgical patients; predicts acute kidney injury, respiratory failure, and in-hospital mortality using only 16 variables
- Demonstrated strong predictive performance with mean AUROCs ranging from 0.82 to 0.91
- Prolonged anesthesia time and low serum albumin identified as key shared predictors of complications
An artificial intelligence model capable of predicting multiple postoperative complications in an integrated manner—similar to the clinical reasoning of experienced physicians—has been developed by researchers at Seoul National University Hospital (SNUH). Using only 16 preoperative clinical variables, the model simultaneously predicts acute kidney injury (AKI), postoperative respiratory failure (PRF), and in-hospital mortality.
Validation results showed that the model outperformed single-task prediction models and demonstrated consistent performance in external validation, indicating strong potential for broad applicability across diverse clinical settings.
The research team, led by Professor Hyun-Kyu Yoonof the Department of Anesthesiology and Pain Medicineand Professor Hyun-Hoon Leeof the Department of Convergence Medicine, developed and validated a multitask machine learning modelbased on data from approximately 80,000 surgical patients, and announced the findings.
Approximately 40% of surgical patientsexperience postoperative complications such as AKI, respiratory failure, or in-hospital death. These complications prolong hospital stays, increase healthcare costs, and negatively affect patients’ and families’ quality of life. Although AI-based models to predict high-risk patients have been developed, most existing models focus on predicting a single complication, limiting their clinical utility.
To address this limitation, the research team selected 16 preoperative variablesstrongly associated with the three complications from electronic health records (EHRs) and developed a multitask gradient boosting machine model (MT-GBM)capable of predicting AKI, PRF, and in-hospital mortality simultaneously. Unlike previous studies that relied on dozens to thousands of variables, this model was designed using a minimal set of routinely available preoperative parameters.
The variables included age, sex, body mass index (BMI), duration of anesthesia, type of surgery (e.g., orthopedics, neurosurgery), American Society of Anesthesiologists (ASA) Physical Status Classification, and laboratory values such as hemoglobin, serum creatinine, albumin, and white blood cell count.
When validated across internal and external cohorts—including SNUH, Nowon Eulji Medical Center, and Korea University Guro Hospital—the model demonstrated strong predictive performance. The mean area under the receiver operating characteristic curve (AUROC) was 0.82 for AKI, 0.91 for postoperative respiratory failure, and 0.89 for in-hospital mortality. Importantly, prediction accuracy remained consistent across all cohorts, supporting the model’s generalizability in different healthcare environments.
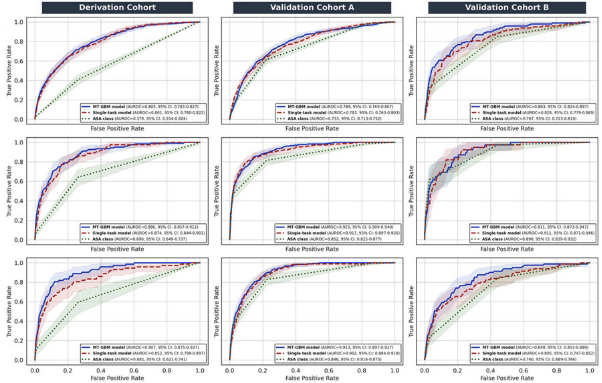
[Figure] Prediction performance (AUROC) for postoperative complicationsThe MT-GBM model (blue) consistently outperformed both single-task prediction models (red) and the ASA Physical Status Classification (green) in predicting AKI, postoperative respiratory failure, and in-hospital mortality across all cohorts.
The MT-GBM model showed higher predictive accuracy than the widely used ASA Physical Status Classificationfor all three complications and consistently outperformed single-task models developed using the same methodology. According to the researchers, this advantage stems from the multitask model’s ability to integrate multiple risk factors simultaneously, mirroring real-world clinical decision-making by physicians.
To further enhance interpretability, the team applied Shapley Additive Explanations (SHAP)to assess the contribution of each variable to the model’s predictions. The analysis revealed that prolonged anesthesia durationand low serum albumin levelswere the most influential shared predictors across all three complications. Longer anesthesia time reflects greater surgical complexity and physiological stress, while low albumin levels indicate poor nutritional status and reduced recovery capacity.
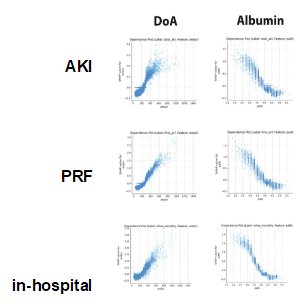
[Figure] SHAP-based analysis of variable contributions to prediction outcomes. Longer duration of anesthesia (DoA) and lower serum albumin levels had a strong impact on the risk of all three postoperative complications.
The researchers noted that the MT-GBM model enables precise preoperative risk stratification, supporting shared decision-making with patients, identification of high-risk individuals, and more efficient allocation of intensive care unit (ICU) resources.
Professor Yoon (Department of Anesthesiology and Pain Medicine; first author) stated, “This study is significant in that we developed a prediction model based on minimal information that can be readily applied at the preoperative assessment stage. In particular, by addressing the interpretability limitations inherent to deep learning models, we have enhanced the reliability of the model’s predictions.”
Professor Lee (Department of Convergence Medicine; corresponding author) added, “The consistent performance of the same AI model across multiple institutions provides compelling evidence that artificial intelligence can be effectively implemented in real-world clinical practice. We plan to further develop this model into a patient-specific preoperative risk prediction tool integrated with electronic health record systems.”
The study was published in the international journal npj Digital Medicine(Impact Factor: 15.1).

[From left]Professors Hyun-Kyu Yoon (Department of Anesthesiology and Pain Medicine) and Hyun-Hoon Lee (Department of Convergence Medicine)