Confirmation of Possibility of Predicting Prognosis of Lou Gehrig's Disease Based on Chest CT
- Analysis of Chest CT of 261 Lou Gehrig's Disease Patients Using Deep Learning Technology... Measurement of Lung and Respiratory Muscle Volume
- Lung and Respiratory Muscle Volume Index: Possible to Evaluate Prognosis of Lou Gehrig's Disease with Accuracy Similar to Existing Tests
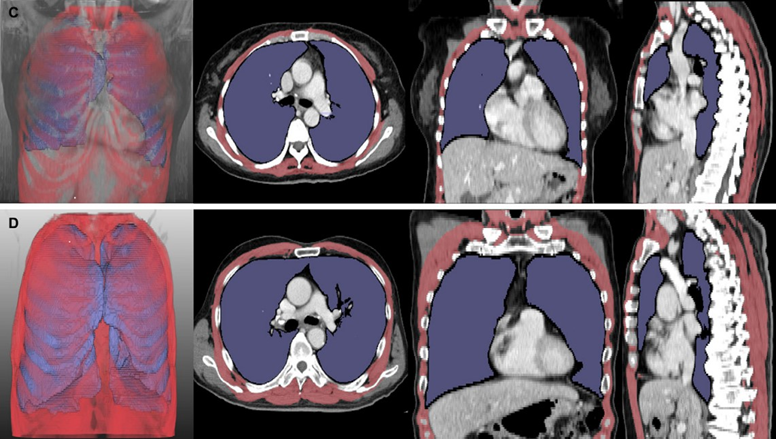
[Figure] Chest CT analysis of patients with Lou Gehrig's disease: Patients with lower lung volume index (LVI, purple) and respiratory muscle volume index (RMI, red) had shorter survival periods than those with higher LVI and RMI (5 months for Picture C vs. 43 months for Picture D).
The respiratory function of patients with Lou Gehrig's disease is primarily assessed using spirometry; however, the accuracy of this test tends to be low for those with weak oral-facial muscles. Researchers at Seoul National University Hospital (SNUH) have developed a new index for testing by analyzing lung and respiratory muscle volume in chest CT images through deep learning technology. This image-based index was found to significantly correlate with disease stage and patient survival. It is anticipated that this new method will address the limitations of existing tests.
A joint research team led by Professors Choi Seok-Jin and Sung Jung-Joon (Dr. Kim Jong-Su) from the Department of Neurology at SNUH, along with Professors Park Chang-Min and Choi Kyu-Sung from the Department of Radiology at SNUH, announced on June 23rd that they confirmed their findings by analyzing chest CT images of 261 patients with Lou Gehrig's disease.
Lou Gehrig's disease is a fatal neurodegenerative disease that gradually destroys motor neurons in the brain and spinal cord. As the disease progresses, even the respiratory muscles become paralyzed, and death from respiratory failure occurs 3 to 4 years after onset. Therefore, patients with Lou Gehrig's disease regularly measure their respiratory function through a spirometry test (a test that measures the amount of air that can be forcefully exhaled after deeply inhaling with a measuring device in the mouth) and decide on an appropriate treatment plan based on the test results.
However, the accuracy of this test was low for patients with impaired oral and facial muscles and dysarthria (a disorder which leads to inaccurate speech and pronunciation), so a new respiratory function test method was needed to replace it.
Therefore, the research team developed the lung volume index (LVI) and respiratory muscle volume index (RMI)*, which use deep learning software to indicate the degree of lung and respiratory muscle atrophy in patients with Lou Gehrig's and show any correlative relationship with the length of patients’ survival periods.
*Lung and Respiratory muscle volume (㎤) divided by the square of the height (㎡)
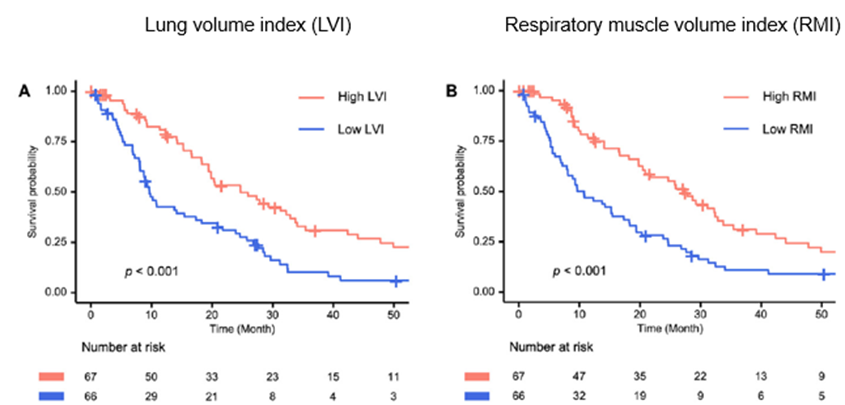
[Graph] Groups with low lung volume index (LVI) and respiratory muscle volume index (RMI) required tracheostomy or experienced death earlier than groups with high LVI and RMI
As a result, the lung and respiratory muscle volume index were found to significantly decrease as the stage of the disease (stages 1 to 4) increased. Moreover, patients with low LVI and RMI exhibited more severe lung and respiratory muscle atrophy and reached the point of tracheostomy or death sooner than those with high indices.
Additionally, statistical analysis indicated that the lung and respiratory muscle volume index can assess patient prognosis with a level of accuracy similar to that of existing spirometry methods. The same trend was observed even among patients with dysarthria. It suggests that the image-based index developed by the research team could potentially replace spirometry in evaluating respiratory function in patients with Lou Gehrig's disease, a condition where evaluating respiratory function is often challenging.
"This study is the first to demonstrate the prognostic value of both qualitative and quantitative imaging indices through deep learning analysis in a large-scale ALS cohort," said Professor Choi Kyu Sung (Department of Radiology, corresponding author).
Professor Choi Seok-Jin and Dr. Kim Jong-Su (Neurology, joint first author) said, "Based on these results, integrating imaging data into clinical practice for Lou Gehrig’s disease could become an effective means to support diagnosis and guide treatment decisions."
The results of this study were recently published in the international academic journal ‘Radiology(IF 15.2)’
[Pictures] Prof Choi Seok-Jin, Dr Kim Jong-Su, and Prof Sung Jung-Joon from SNUH Department of Neurology and Prof Park Chang-Min and Prof Choi Kyu Sung from SNUH Department of Radiology