Patients with advanced cancer have varying survival rates depending on their coping strategies, even when at the same cancer progression stage
- Seoul National University Hospital proved that the interactive relationship between proactive positivity and depression affects survival rate
- Patients with low proactive positivity and comorbid depression have a 4.63 times higher risk of death within one year
The published research results show that “Even in the same disease stage, survival varies depending on how you cope.” A research team at Seoul National University Hospital (SNUH) analyzed the effect of the interaction between ‘depression’ and ‘proactive positivity’ on the 1-year survival rate in patients with advanced cancer and found that patients with low coping strategies and depression had a 4.63 times higher risk of death than the reference group. This suggests that a patient’s psychological resilience and proactive positivity coping strategies can have a greater impact on survival than the mere presence or absence of depression.
On June 19, a research team led by Professor Yun Young-Ho of the Department of Family Medicine at SNUH (corresponding author), Professor Yun Je-Yeon of the Office of Education and Human Resources Development (concurrently with the Department of Psychiatry, joint first author), and Professor Jung Ju Youn of the Department of Tourism & Wellness at Hankuk University of Foreign Studies (joint first author) announced the results of a prospective secondary analysis conducted on 144 patients with advanced cancer who participated in an early palliative care clinical trial at 12 general hospitals nationwide.
Patients who reach terminal stages after being diagnosed with cancer are prone to psychological distress, such as loss of self, fear of death, and confusion about the meaning of life. In fact, it is known that approximately 30% of all cancer patients experience clinically significant levels of depressive symptoms, which can affect not only the quality of life but also survival prospects. The research team aimed to empirically investigate how these mental health factors influence survival outcomes.
All study subjects were stage 4 or high-risk patients who had relapsed after treatment, with a predicted survival period of less than one year. The patients had various types of cancer, including lung, liver, pancreatic, colon, stomach, and breast cancer. The research team assessed the psychological resilience of these patients using key items from the Smart Health Management Strategy Tool (SAT-SF). This strategy presented the following components: ▲Positive restructuring, ▲Active problem solving, and ▲Experience sharing & relationship-centered behavior. These components are collectively defined as a ‘positive coping strategy’ (Proactive Positivity). This approach helps patients maintain emotional stability and take active steps to reorganize their lives during crises. The research team divided the strategy level using a baseline SAT-SF score of 66.66 points, and classified depressive symptoms as moderate or severe depression when a patient’s PHQ-9 score was 10 points or higher. The ECOG-PS index was utilized to evaluate the patients' physical function level.
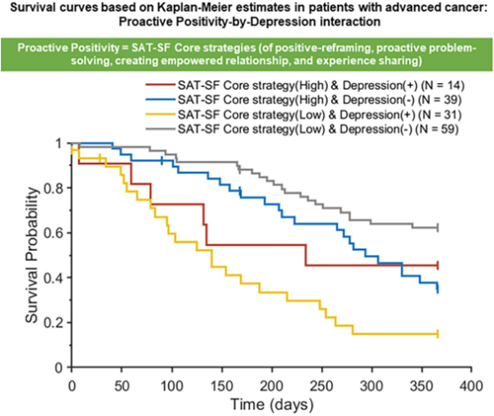
[Graph] Kaplan–Meier survival curve: The one-year survival rate was lowest in patients with low positive coping strategies and depression (yellow), while in patients with high coping strategies (red, blue), there was little difference in survival rate depending on the presence or absence of depression.
The research team divided the patients into four groups based on the level of proactive positivity (high/low) and the presence or absence of depression (yes/no), and compared their 1-year survival rates. As a result, in the ‘low proactive positivity patient group’, the risk of death was 4.63 times higher when depression was present than when it was not (aHR=4.63, 95% CI: 2.54–8.43, p<0.001). On the other hand, in the ‘high proactive positivity patient group’, no significant difference in the risk of death was observed depending on the presence or absence of depression.
These results show that the effect of depression on decreased survival rate may vary depending on the nature of the patient's coping strategy. In particular, while there was a statistically significant association between depression and decreased survival rate in patients with low proactive positivity, the risk of death did not significantly increase in patients with high proactive positivity even if they had depression. This suggests that in patients with advanced solid-tumor cancer with low proactive positivity, it is necessary to more closely evaluate the presence of depression and intervene therapeutically.
Meanwhile, physical function status also had a significant impact on survival rate. Patients with an ECOG-PS score of 2 (self-care is possible but daily life is difficult) had a 2.33 times higher risk of death than patients with scores of 0 to 1 (HR=2.33, 95% CI: 1.25–4.34, p=0.012). In addition, SAT-SF scores tended to decrease over time, confirming the reality that it is difficult to maintain proactive positivity as the disease progresses.
The research team emphasized that how patients perceive and respond to depression itself can be a key factor in determining survival. In fact, patients with high proactive positivity tended to be less negatively affected by depression. This supports the need for interventions that enhance psychological resilience to improve the survival rate of terminally ill cancer patients.
Professor Jung Ju Youn (Department of Tourism & Wellness at Hankuk University of Foreign Studies) said, “This study is the first to statistically prove that patients with low positive coping strategies and comorbid depression have the highest risk of death.”
Professor Yun Je-Yeon (SNUH, Office of Education and Human Resources Development) explained, “The results show that mental health interventions that assess and improve depression levels and coping strategies together can contribute to improving patients’ survival rates.”
Professor Yun Young-Ho (SNUH, Department of Family Medicine) emphasized, “These results are empirical evidence that support the results of the early palliative care clinical trial published in JAMA Network Open from a psychosocial perspective and suggest the need for mental health intervention based on a smart health management strategy.”
This study was conducted with the support of the Ministry of Health and Welfare's Health and Medical R&D Project, the National Research Foundation of Korea, and the Ministry of Science and ICT, and the results were published in the latest issue of the international academic journal BMC Psychiatry.

[Pictures from left] Professor Yun Young Ho of the Department of Family Medicine at SNUH, Professor Yun Je-Yeon of the Education and Human Resources Development Center, and Professor Jung Ju Youn Joo-Yeon of the Department of Tourism & Wellness at Hankuk University of Foreign Studies