High-risk group for bleeding after coronary artery intervention has a 3.7 times higher risk of death
Seoul National University Hospital presented results from a decade of follow-up observation of 320,000 individuals who underwent coronary artery intervention.
- 1 in 5 people are in a high-risk group for bleeding, having respectively 3.1 times and 2.5 times higher risk of bleeding and ischemic events.
A large-scale study analyzing the long-term prognosis of patients at a high risk of bleeding after coronary artery intervention was published. The study found that these patients experienced more long-term adverse effects compared to others and had a 3.7 times higher risk of death. This suggests that tailored treatment strategies will likely be necessary to improve the prognosis of this high-risk bleeding group.
On August 27th, a research team led by Professors Kim Hyo-Soo, Park Kyung Woo, and Kang Jeehoon (Clinical Instructor Yun Junpil) from the Department of Cardiology at Seoul National University Hospital announced the results of a study in which they analyzed the clinical characteristics and long-term prognosis of a high-risk group for bleeding based on data from the National Health Insurance Service of approximately 325,000 patients who underwent percutaneous coronary intervention from 2009 to 2018.
Acute coronary syndrome is a fatal disease that causes angina and myocardial infarction. For treatment, coronary angioplasty is performed to widen the narrowed coronary artery. After the procedure, antiplatelet drugs are essential to prevent recurrence, but if a person with an underlying disease takes these drugs for a long time, bleeding side effects may occur.
In 2019, an international research consortium published the definition and criteria for the ‘high-risk group for bleeding’ to identify patients at risk for bleeding side effects of antiplatelet agents after percutaneous coronary intervention. The high-risk group for bleeding refers to patients with 'one major standard' such as long-term use of antiplatelet agents, severe to end-stage renal disease, severe anemia, liver cirrhosis, cancer, cerebral hemorrhage, etc., or 'two minor standards' including an age ≥75 years, moderate renal disease, mild anemia, long-term use of steroids or nonsteroidal anti-inflammatory drugs, etc.
However, there has been a lack of research to verify the definition and criteria of high-risk bleeding groups by analyzing the size, clinical characteristics, and long-term prognosis of a large patient group. After the research team analyzed approximately 325,000 domestic patients who underwent coronary artery intervention, one in five patients was found to be in the high-risk group for bleeding.
After following up with all patients for 10 years, researchers found that the high-risk group for bleeding had a 3.12-fold higher risk of hemorrhagic events and a 2.5-fold higher risk of ischemic events compared to other patient groups. Additionally, the high-risk group had a 3.73-fold higher risk of death from all causes. This means that the high-risk group for bleeding faced a greater long-term risk of clinical adverse effects and death following coronary artery intervention.
*Ischemic events: myocardial infarction, ischemic stroke, etc.
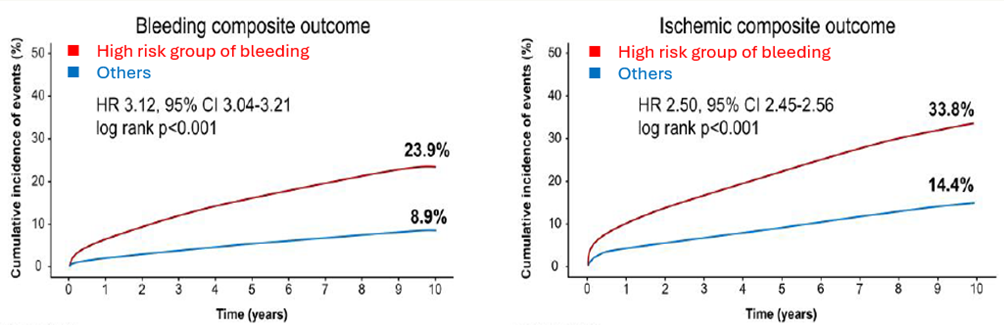
[Graph] The high-risk group for bleeding had a higher risk of both bleeding and ischemic events than the other patient groups during the 10-year follow-up
In addition, the research team analyzed the major and minor standard for classifying the high-risk group for bleeding. The major standard were severe anemia (24.2%), long-term use of antiplatelet agents (22.2%), chronic bleeding (11.0%), and severe-end-stage renal disease (9.1%). Minor standard included age 75 years or older (50.5%) and mild anemia (42.1%). In particular, the annual average incidence of bleeding events within 1 year after coronary artery intervention was 5.5% for instances of patients with 1 major standard and 2.9% with 1 minor standard.
Professor Park Kyung Woo of the Department of Cardiology said, “This study confirmed that 20% of patients undergoing percutaneous coronary intervention are at high risk for bleeding with a poor long-term prognosis.” He added, “In order to improve their survival rate, we need to carefully manage comorbidities and develop a tailored drug treatment strategy that precisely adjusts the duration of antiplatelet therapy or lowers the dose.”
The results of this study were published in the latest issue of the ‘European Heart Journal (IF;37.6)’.

[Pictures from left] Professors Kim Hyo-Soo, Park Kyung Woo, Kang Jeehoon and Clinical Instructor Yun Junpil from the Department of Cardiology at Seoul National University Hospital