SNUH opens customized treatment pathway by optimizing transcatheter pulmonary artery valve implantation.
- Successful optimized treatment through the patient-tailored model using 3D printing and in vitro mock circulation device
- Finding the optimal transcatheter pulmonary artery valve size and insertion location...Increase of success rate and minimization of side effects
Seoul National University Hospital recently succeeded in optimizing transcatheter pulmonary artery valve implantation for a 24-year-old patient with Tetralogy of Fallot with pulmonary artery valve regurgitation using a patient-specific model using 3D printing and an in vitro mock circulatory device. This treatment method helped determine the optimal size and insertion location for percutaneous pulmonary artery stent valves in various sizes and shapes of the right ventricular outflow tract (the inlet of the pulmonary artery, the blood vessel that goes from the right ventricle to the lungs). Thus, it is expected that the success rate of transcatheter pulmonary artery valve implantation can be increased and side effects can be minimized.
Transcatheter pulmonary artery valve implantation is a minimally invasive treatment that improves pulmonary artery stenosis or regurgitation by inserting an artificial pulmonary artery valve through the femoral vein without making a chest incision.
The heart consists of two atria and two ventricles and has four valves (aortic valve, pulmonary valve, tricuspid valve, and mitral valve) that help prevent blood from flowing back between each part. The ‘pulmonary artery valve’ located between the right ventricle and the pulmonary artery plays the role of preventing the blood from returning to the right ventricle after the right ventricle pumps blood into the lungs. Pulmonary artery valve disease is a disorder that occurs concerning the opening and closing mechanism of the valve.
In the case of patients who have undergone pulmonary artery valve plastic surgery due to congenital right ventricular outflow tract anomalies such as Tetralogy of Fallot, as valve function declines with age and regurgitation occurs, it can cause the right ventricle to enlarge or the valve to narrow, resulting in severe stenosis. If this progresses to heart failure, it can become dangerous.
To prevent this, thoracotomy/open heart surgery has been performed to open the chest, erect the heart, and replace the pulmonary artery valve. However, in the case of reoperation, pain and aftereffects are significant, and as the number of reoperations increases, the risk of complications increases, so the development of a treatment alternative to surgery is urgently needed.
Accordingly, the Pediatric Heart Center team began performing ‘percutaneous pulmonary artery valve implantation’ on patients with pulmonary artery regurgitation. This treatment is a procedure that improves pulmonary artery stenosis or regurgitation by percutaneously inserting an artificial valve without surgery to expand the narrowed valve.
For successful transcatheter pulmonary artery valve implantation, it is important to determine the optimal size and insertion location of the transcatheter pulmonary artery stent valve in right ventricular outflow tract diseases that vary in size and shape depending on each patient.
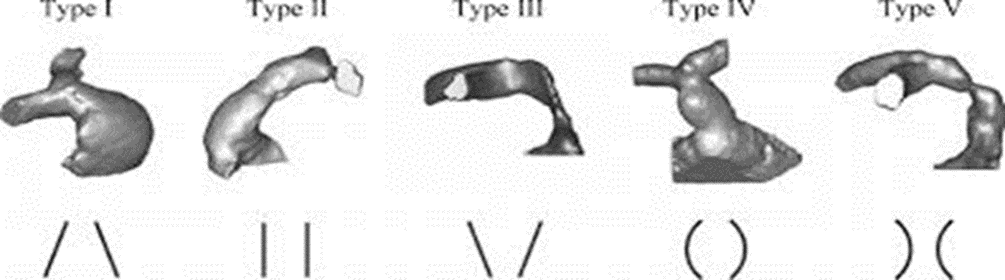
[Image] Various right ventricular outflow tract shapes in pulmonary artery valve disease (Source: Circ Cardiovasc Imaging. 2014;7:182-189)
The shape of the right ventricular outflow tract is divided into △Type 1 Pyramidal △Type 2 Straight △Type 3 Reverse Pyramidal △Type 4 Convex △Type 5 Concave. The pulmonary artery stent valve has the characteristic of adapting to various shapes of the right ventricular outflow tract. Therefore, when performing transcatheter pulmonary artery valve implantation, the size and insertion location of the pulmonary artery stent valve must be varied according to the various sizes and shapes of each patient's right ventricular outflow tract to improve the success rate of the treatment.
In addition, heart and blood vessel segmentation is performed based on CT or MRI images of patients with complex cardiac anomalies, and an STL (stereolithography) file is created. Afterwards, it is important to accurately model complex anatomical structures using 3D printing and perform customized treatment for patients using in vitro mock circulation.
The patient treated this time was a tetralogy of Fallot patient (male, 24 years old) who had pulmonary artery valve regurgitation accompanied by right ventricular dilatation and functional decline after undergoing complete correction surgery. Tetralogy of Fallot is a congenital heart disease that has four anatomical abnormalities: right ventricular outflow tract stenosis, ventricular septal defect, aortic riding, and right ventricular hypertrophy.

[Photo] A stent valve inserted into a customized right ventricular outflow tract taken with an endoscopic camera.

[Photo] In vitro mock circulation device
Seoul National University Hospital's team led by Professor Kim Ki-Beom of the Department of Pediatrics, Lee Hwal of the Department of Pediatric Radiology, and Lim Hong Gook of the Department of Pediatric Thoracic Surgery created this patient's customized right ventricular outflow tract similar to the actual tissue using cardiac computed tomography (CT) images using 3D printing then connected with in vitro mock circulation device.
Afterwards, percutaneous pulmonary artery stent valves of various sizes were inserted into various locations in the patient-specific right ventricular outflow tract to operate in vitro mock circulation. Next, the research team checked the condition of the inserted stent valve with an attached endoscopic camera and tried to find a treatment method optimized for the patient.
Through this, the optimal percutaneous pulmonary artery stent valve size and insertion location were determined, and a 22mm percutaneous pulmonary artery stent valve implantation was performed on the 2nd of November.
As a result, the patient was treated successfully and was discharged in good health on the 6th. The patient is in good health without any special side effects.
Professor Kim Ki Beom (Department of Pediatrics) said, “Determining the optimal size and insertion location of the percutaneous pulmonary artery stent valve in the right ventricular outflow tract, which has various sizes and shapes depending on the patient, is the key to the success of the procedure.”. “If we determine the optimal size and insertion location of the percutaneous pulmonary artery stent valve in right ventricular outflow tracts of various sizes and shapes through this treatment method we will be able to increase the success rate of percutaneous pulmonary valve implantation and minimize side effects,” he added.
This study was conducted with funds from [Lee Kun Hee Foundation: Pediatric Cancer and Rare Disease Overcoming Project].