Patients who quit smoking after PCI have similar treatment outcomes to non-smokers.
- The Seoul National University Hospital research team announced the results of a clinical study analyzing 74,471 percutaneous coronary intervention (PCI) patients.
- If you smoke for more than 20 pack-years, the smoking cessation effect disappears.
[Photo] SNUH Department of Cardiovascular, Professor Han Jung-Kyu
A domestic research team published the results of a large-scale clinical trial that looked at the smoking status and treatment outcomes of patients who had percutaneous coronary intervention (PCI). Nonsmokers had superior treatment outcomes than smokers after the surgery, while ex-smokers had treatment outcomes similar to nonsmokers.
Patients who started smoking cessation after the procedure had treatment results similar to non-smokers if their smoking history did not exceed 20 pack-years, but treatment results similar to smokers if their smoking history exceeded 20 pack-years.
[Glossary of terms] pack-years: The product of the number of cigarettes smoked per day (pack) and the period of smoking (years). For example, if you smoke 1 pack a day for 20 years, or 2 packs a day for 10 years, this is converted into 20 pack-years of smoking.
Professor Han Jung-Kyu's team at Seoul National University Hospital's Department of Cardiology (Professor Ki You-Jeong at Uijeongbu Eulji University Hospital and Professor Han Kyungdo at Soongsil University) analysed the smoking status of 74,471 patients who received PCI treatment between 2009 and 2016 using a nationwide database from the Korean National Health Insurance System. As a result, the following facts were confirmed and published in the ‘European Heart Journal (EHJ IF: 39.3)’, the most authoritative journal in the cardiovascular field.
Angina, which produces chest pain during activity, or myocardial infarction, which destroys the heart muscle due to an acute blood flow blockage, occur when the coronary artery that feeds blood flow to the heart muscle narrows. In order to treat this, stent implantation or balloon dilatation can be used as part of PCI to enlarge the stenotic coronary artery.
Smoking is a well-known significant risk factor for individuals suffering from cardiovascular disease. However, there has been no research in large-scale population-based studies on the effect of smoking on treatment outcomes after coronary artery surgery in patients treated with the latest medical technologies, such as drug-eluting stents.
The impact of smoking cessation following PCI, in particular, on the results of treatment outcomes is unknown. It is not feasible to evaluate treatment outcomes by randomly allocating patients who have had coronary artery surgery to either a smoking group or a smoking cessation group due to ethical concerns. Therefore, large-scale population-based studies are important to determine the effects of smoking. Considering this, the researchers used data analysis from the Korea National Health Insurance Corporation to carry out this investigation.
First, 74,471 people who underwent a health checkup within 1 year after undergoing a coronary artery procedure and had data on their smoking status were divided into ▲non-smokers ▲smokers ▲ex-smokers (smokers who have smoked but quit smoking at the time of the checkup) according to their smoking status at the time of the health checkup. After analyzing the treatment outcomes after coronary artery surgery in the three groups (median observation period of 4 years), the risk of major adverse cardiac and cerebrovascular events (MACCE) in smokers was 20% higher than in non-smokers. In the case of former smokers, a similar risk of occurrence was observed as that of non-smokers.
In other words, the research team explains that even with the latest coronary artery treatment, smoking has a negative effect on treatment outcomes.
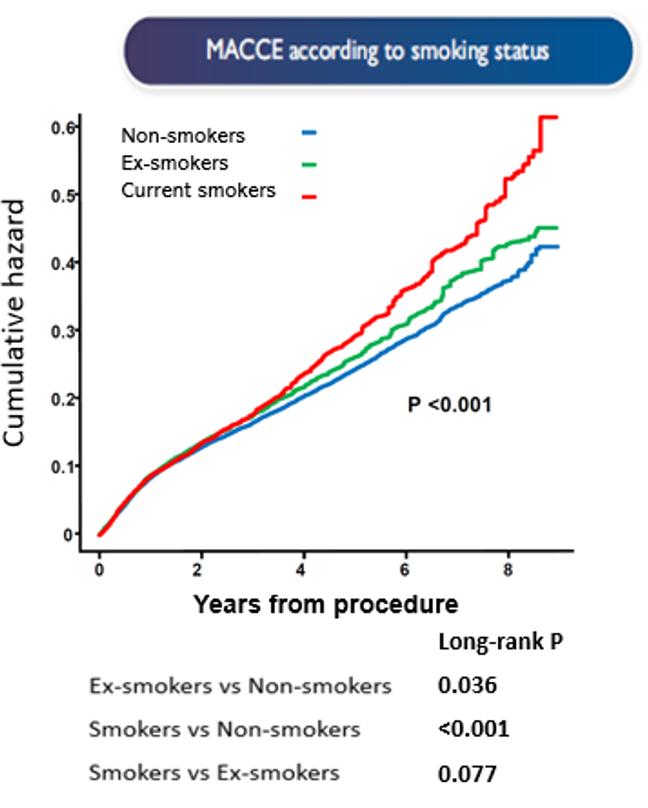
[Figure] Risk of major adverse cardiac and cerebrovascular event (MACCE) according to smoking status after the procedure. Smokers were observed to have a 20% higher risk than non-smokers.
Subsequently, the researchers divided 31,887 patients who underwent health checkups before and after coronary artery surgery (median interval between two health checkups: 628 days) into three groups according to changes in smoking status, ▲non-smoker (non-smoker → non-smoker) ▲continuous smoker (smoker → smoker) ▲non-smokers (smoking → non-smoker) and analyzed the data.
As a result, in patients with a smoking history of less than 20 pack-years, the risk of major adverse cardiac and cerebrovascular event (MACCE) was statistically similar to that of non-smokers if they quit smoking after PCI. On the other hand, in patients with a smoking history of more than 20 pack-years, the risk of major cardiovascular events was similar to that of continuous smokers even if they quit smoking. This is understood to occur when the accumulated amount of smoking exceeds a certain level and causes irreversible damage to the heart muscle.
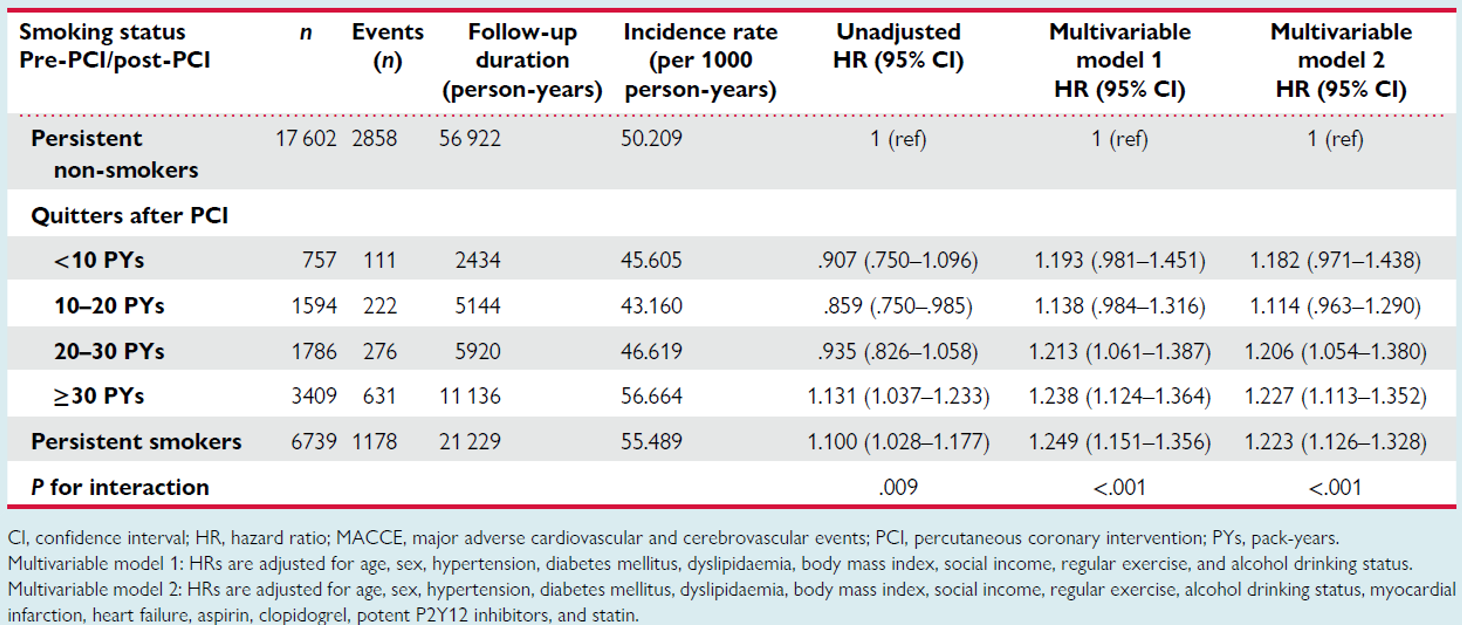
[Table] Risk of major adverse cardiac and cerebrovascular event (MACCE) according to smoking status before and after the procedure. Smokers with less than 20 pack-years of smoking had a risk that was statistically similar to that of non-smokers.
Furthermore, the researchers separately analysed 28,366 patients who underwent coronary artery surgery (CPI) for myocardial infarction. As a result, as shown in the overall patient group, smokers had a 15% higher risk of major cardiovascular events compared to non-smokers, and ex-smokers had a risk similar to that of non-smokers. However, in patients who underwent coronary artery surgery for myocardial infarction, no significant reduction in the risk of major adverse cardiac and cerebrovascular event (MACCE) was observed even if they quit smoking after the procedure.
The research team estimates that this was either not statistically significant due to the insufficient number of patients being analysed, or it was a result of myocardial infarction synergizing with the damage to the heart muscle accumulated from past smoking, causing greater irreversible damage.
Professor Han Jung-Kyu said, “This study proved through a large-scale population-based study that smoking has a negative effect on treatment outcomes even in patients receiving the latest coronary artery treatment. “, “However, if the smoking history is less than 20 pack-years, it is important to observe treatment results similar to those of non-smokers if the patient quits smoking after the procedure.” He went on, "In particular, doctors and patients should pay attention and effort to quickly implement active smoking cessation, as even smokers have a window of opportunity of about 20 pack-years to achieve as good treatment results as non-smokers."
Professor Han continued, “On the other hand, several previous studies have reported 'the smoker's paradox’ that patients with myocardial infarction who smoke have better treatment outcomes than non-smokers, but this large-scale population-based study showed that this is not the case.” "Furthermore, the fact that the positive effect of smoking cessation after the procedure was not noticeable in patients who had already suffered a myocardial infarction shows the need to quickly quit smoking before a myocardial infarction occurs.”
"Randomised clinical trials on this topic are difficult to conduct due to ethical issues, so this is an area where large-scale population-based research is especially valuable," he said, highlighting the study's significance.