SNUH Palliative Care and Clinical Ethics Center publishes 2021 business report
- In 2021, there was an average of 147 patients per month in palliative care: there has been an increase in referrals for surgical and non-cancer diseases
- As a result of a retrospective cohort analysis of cancer patients who died between 2019 and 2020: Emergency room deaths doubled
- Inconvenience of using medical treatment for severely ill patients in during COVID-19↑, choice of methods for using and caring in medical institutions↓
On the 13th of April, SNUH Palliative Care and Clinical Ethics Center (Centre Director Kim Beom-Seok) announced that it had published its ‘2021 Business Report’ which outlines major business activities and achievements.
The Palliative Care and Clinical Ethics Center was opened in 2018 with the aim of contributing to the dignified life of patients, a first among domestic medical institutions. It provides palliative care and clinical ethics support services, including an advisory hospice, and directs the ethical committee of our medical institution’s deliberation, administration, education, and policies.
In addition, it provides guidance on life-sustaining treatment plans, referrals, psycho-emotional support, and socio-economic support in consideration of the patient's symptoms, the psycho-emotional state of the patient and their family, family structure, care type, and economic problems,.
According to the business report, a total of 1,759 palliative care patients were referred to the center in 2021, with a monthly average of 147, showing a steady increase from 90 in 2018, 113 in 2019, and 122 in 2020.
837 (47.6%) patients were referred from outpatient care, 651(37%) from wards, 130 (7.4%) from the emergency room, and 141 (8%) from the intensive care unit.
By department, haematology oncology had the most requests with 1,076 patients (61.2%). Compared to 2020, the number of requests from emergency medicine, gastroenterology, respiratory medicine, neurosurgery, and other surgical and non-cancer disease departments increased.
The center paid attention to the situations where many patients faced a lonely death. It is due to the difficulty of visiting medical institutions and taking care of hospitalized family members to ensure the safety of patients, their families, and medical staff amid the COVID-19 situation.
In fact, a retrospective cohort analysis was conducted on 1,456 cancer patients who died between 2019 and 2020 in order to understand what kinds of conditions patients face at the end of their life in advanced general hospitals in the era of COVID-19.
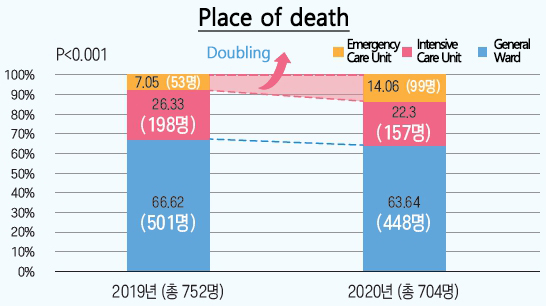
The analysis found that the number of deaths in emergency departments more than doubled in 2020 compared to 2019. In addition, it was found that the rate of aggressive medical interventions when providing life-sustaining treatment as well as of uncomfortable symptoms experienced by terminal patients increased significantly.
In particular, delirium before death, use of vasopressors, and cardiopulmonary resuscitation (CPR) performed one month before death increased even more in places with strict access restrictions, such as multi-person rooms or intensive care units. This shows that end-of-life patients are facing a death that is far from a comfortable and dignified death.
In addition, the center paid attention to problems in the care system for the severely ill caused by COVID-19. Qualitative research analysis was conducted after in-depth interviews with 9 healthcare workers including those employed in home-care/home-nursing, the emergency room of a tertiary general hospital, paramedics, hospice, and nursing hospital.
As a result, it was found that severely ill patients not only experienced inconvenience in using medical care due to the COVID-19 situation but also had fewer options for which medical institutions and care methods they used. In addition, it was confirmed that cases of inhumane end-of-life care and death have increased due to the prioritization of quarantine measures.
To solve this problem, the center produced an educational video to improve the quality of end-of-life care and participated in a home-type hospice pilot project. In addition, it trained bereaved-family-counselling specialists and provided integrated services from terminal care to death preparations and bereavement after death.
In particular, the center held a symposium last year to discuss the problems experienced by medical staff struggling to apply the Life-sustaining Medical Decision Act and find the right direction to take in certain circumstances, a grey area. Additionally, it said that it provided systematic clinical ethics support for various ethical issues surrounding patients, such as continuation or discontinuation of treatment, life-sustaining treatment, organ transplantation, quality of life of patients, and conflicts between medical staff and patient-family members.
Kim Byung-Kwan, deputy director of medical treatment, said, “2021 was a year in which we expanded the scope of palliative care and clinical ethics treatment, and educated medical personnel inside and outside the hospital through a variety of topics and methods. We will strive to become a model for practicing 'value-oriented medical care' in Korea, encompassing medical treatment, education, and research," he said.
Kim Beom-Seok, head of the Center (and Professor of Hematology and Oncology) said, “This business report delineates the progress of the center’s cooperative activities both internally and externally and its efforts to respond to the COVID-19 situation.” He also added “We hope that through our work, we can create a solid foundation for promoting 'human-like medical care' in every field.”
This project report has been distributed to institutions specializing in palliative care and medical institution ethics committees nationwide and can be downloaded and viewed from the Seoul National University Hospital Palliative Care and Clinical Ethics Center website (http://hospice.snuh.org/).